Article / Publication
Source:
Key Takeaway: Real-world data from the German/Austrian Prospective Diabetes Follow-Up Registry showed real-time continuous glucose monitoring was associated with a higher percentage of Time-in-Range and improved metabolic stability as compared to intermittent scanning continuous glucose monitoring.
Learn MoreSource:
Key Takeaway: A recent systematic review and meta-analysis of 15 randomized controlled trials involving 2,461 patients showed greater improvement in mean hemoglobin A1c, time in target range, and time above range with use of real-time continuous glucose monitoring as compared to intermittently scanned continuous glucose monitoring.
Learn MoreSource:
Key Takeaway: In a Medicaid population of youth with Type 1 Diabetes, uninterrupted continuous glucose monitoring (CGM) use was associated with improvements in hemoglobin A1c. Interruptions in use—primarily due to gaps in insurance coverage of CGM—were associated with increased hemoglobin A1c, supporting initial and ongoing CGM coverage in high-risk, publicly insured demographics.
Learn MoreSource:
Key Takeaway: Recent data from a prospective, randomized study conducted by Intermountain Health suggests that real-time CGM can reduce healthcare utilization and decrease the overall cost of care compared to SMBG. Participants reported that real-time CGM data were helpful in modifying their nutrition, physical activity, stress, and medication adherence.
Learn MoreSource:
Key Takeaway: In a 16-week trial funded by the NIDDK and Tandem Diabetes Care, 101 children ages 6-13 with type 1 diabetes were randomized to a closed-loop system of insulin delivery (n=78) or the control group (n=23) where patients used a sensor-augmented insulin pump. Children using the closed-loop system, consisting of a t:slim X2 insulin pump with Control-IQ technology and a Dexcom G6 CGM, saw a significant time in range (TIR) improvement (target 70-180 mg/dL) from 53% at baseline to 67% (equivalent to 3.4 more hours per day; p<0.001) at the end of the study. The control group saw a smaller TIR increase from 51% at baseline to 55% at the end of the study. Notably, TIR increased most significantly overnight with children reaching 80% overnight TIR compared to 54% in the control group. The treatment effect was evident in the first month and appeared consistent over 4 months. Control-IQ technology demonstrated benefits across a broad range of baseline characteristics and proved easy to use for children and their parents.
Learn MoreSource: Journal of the American Medical Association
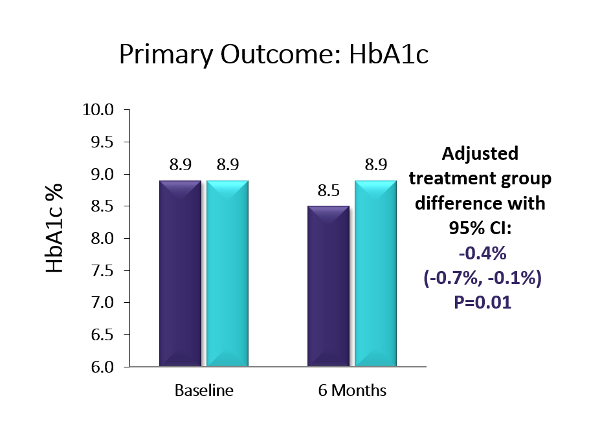
Key Takeaway: Six-month, multicenter, randomized controlled trial using the Dexcom G5. The baseline population had diverse racial/ethnic backgrounds (38% Hispanic or non-white), high baseline HbA1c levels, and 41% had public health insurance. The trial showed a 0.4% A1c advantage in favor of CGM over BGM (p=0.01; baseline: 8.9%). Moreover, more than twice as many in the CGM group as compared to the BGM group achieved an A1c reduction ≥0.5% (44% vs. 21%, p=0.005) and over four-times as many participants in the CGM group vs. the BGM group saw an A1c reduction of ≥1% (25% vs. 6%, p=0.003). The CGM group also saw a 1.7 hour/day advantage vs. BGM on time-in-range (70-180 mg/dl) (p<0.001). Over two-thirds of the CGM group were using CGM at least five days/week by the end of the six-month study – the highest CGM use observed for adolescents in a study to date. Moreover, the CGM group reported significantly higher glucose monitoring satisfaction, measured via the Glucose Monitoring Satisfaction Survey score, at 26 weeks than the BGM group . Newer models of CGM devices that eliminate fingerstick calibration should lead to improved wearability and glycemic control even beyond the measured benefits observed in this trial. Improved glycemic control early in diabetes duration may prevent diabetes complications later in adulthood, making CGM an attractive option for this population.
Source: Journal of the American Medical Association
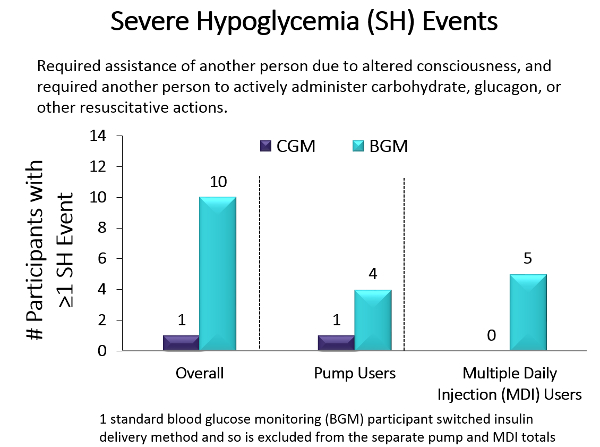
Key Takeaway: Older populations are more prone than younger populations to severe hypoglycemic episodes, which in turn contribute to dementia, risk of falls, glycemic variability, and mortality. To study whether CGM could reduce hypoglycemia incidence, Pratley and colleagues performed a randomized clinical trial that compared the effect of CGM (n = 103) with BGM (n = 100) in older adults (median age, 68 years) with type 1 diabetes in 22 diabetes centers across the US. The primary outcome was reduction in hypoglycemia (glucose <70mg/dL) over 6 months. Results showed that the median time in hypoglycemia was reduced from 73 minutes to 39 minutes per day in the CGM group compared with no change (from 68 minutes to 70 minutes per day) in the BGM group, an adjusted between group reduction of 27 minutes per day (95% CI, −40 to −16 min/d). Additionally, the median percentage of time with blood glucose levels below the range for severe hypoglycemia (glucose <54mg/dL) reached the goal per international guidelines (<14min/d in older adults). Moreover, only 1 severe hypoglycemic event (glucose <54mg/dL) occurred in the CGM group vs 10 in the BGM group, with 5 of those events involving seizure or loss of consciousness. 83% of participants in the CGM group used CGM at least 6 days per week during month 6 and the results did not differ by level of cognitive impairment, education level, or age. In summary, CGM reduced the time spent in the severe hypoglycemic range, which has health care use, mortality, morbidity, and economic benefits.
Announcing a new white paper based on key findings from the Therapeutic CGM Health Care Stakeholder Summit held on November 7, 2019, in Washington, DC. The stakeholder panel included payer and employer leadership along with clinical experts in the field of endocrinology. The purpose was to gather input pertinent to the coverage and application of therapeutic continuous glucose monitoring (CGM) in managed care settings. Clinical evidence supporting the clinical and economic value of rtCGM was presented and the insights of these health care stakeholders were captured en route to formulating coverage policy recommendations for the future. This input is intended to advance the uptake and appropriate coverage of evidence-based health technology interventions by managed care organizations (MCOs) and various payers.
Learn MoreSource: Diabetes Care
Key Takeaways: CGM has emerged as a new standard of care for individuals with insulin-treated diabetes. Two types of CGM systems are now available: real-time CGM (rtCGM) and intermittently scanned (isCGM). rtCGM systems automatically transmit a continuous stream of glucose data to the user, provide alerts and active alarms, and transmit glucose data in real time to a smart phone and/or other display device. The current isCGM system provides the same type of data but requires the user to purposely scan the sensor to obtain information, and it does not have alerts and alarms. Both CGM technologies have significant advantages over self-monitoring of blood glucose; however, differences in the features and capabilities of the two approaches must be considered when guiding patient selection of the system that meets their individual needs.
Learn MoreSource: American Journal of Managed Care
Key Takeaway: The use of CGM is proven to reduce A1C, reduce time spent in hypo- and hyperglycemia and improve time in range (TIR) for Type 1 and Type 2 patients using intensive insulin, defined as multiple daily injections of insulin or getting insulin through an insulin pump. This has resulted in guidelines and recommendations from professional societies such as the ADA recommending CGM as a standard of care for Type 1 and Type 2 patients using intensive insulin. CGM is an important monitoring tool that is best accessed by providers and patients in the pharmacy channel
Learn More