Coverage and Benefit Design

Intended Audience: This activity is designed to meet the educational needs of managed care pharmacy directors, clinical pharmacists, quality directors, medical directors, registered nurses, and other managed health care professionals.
Credit Available: Up to 1.0 credit hour available for nurses (ANCC), pharmacists (ACPE), and physicians (AMA PRA Category 1 Credit™)
Expired
Click Here to Review – CE ExpiredEDUCATIONAL OBJECTIVES
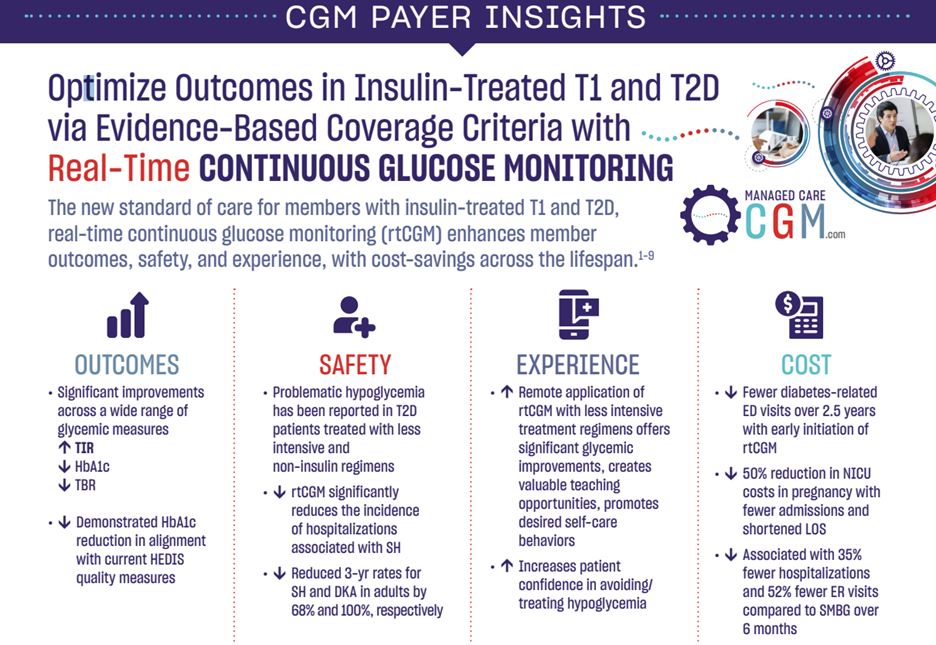
- Review the latest data supporting the use of rtCGM to improve patient outcomes and reduce resource utilization in T1 and T2D
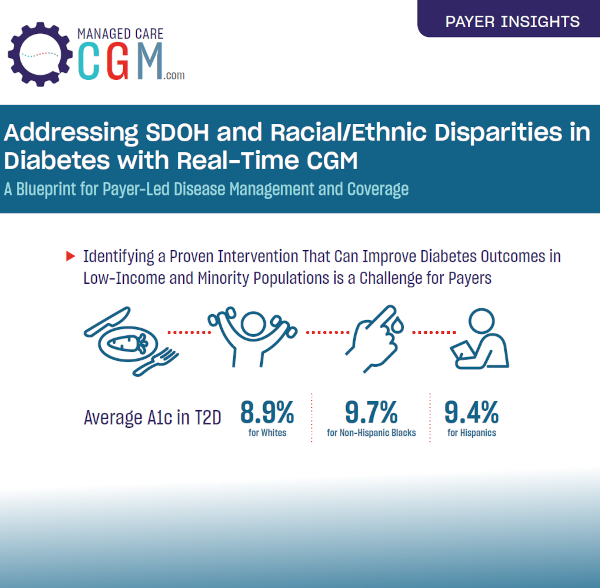
- Assess the impact of social determinants of health (SDOH) on outcomes in diabetes among low-income and racial/ethnic minority populations
- Describe the role of diabetes technology in increasing patient engagement and self-management across diverse member populations of varying age, race/ethnicity, income, and insurance type
- Discuss the positive impact of electronic prior authorization for rtCGM under the pharmacy benefit in terms of provider administrative burden, access, and total cost of care
EXPERT FACULTY

Monica Peek, MD, MPH, MS
Professor of Medicine
Associate Director
Chicago Center for Diabetes Translational Research
The University of Chicago Medicine

Samir Mistry, PharmD, MBA
Vice President of Pharmacy Strategy & Services
Capital Blue Cross

Kelly Close
Founder, The diaTribe Foundation
President, Close Concerns

Dana McCormick, RPh, FMACP (Moderator)
Director of Pharmacy
Blue Cross Blue Shield of Texas
Jointly provided by Impact Education, LLC, and Medical Education Resources.
This continuing education activity is supported by an independent educational grant from Dexcom, Inc.
The National Committee for Quality Assurance (NCQA) is revising its Healthcare Effectiveness Data and Information Set (HEDIS) standardized measures assessing plan performance for 2023. Notably, the 2023 dataset will include a new measure related to diabetes management: the risk-adjusted ratio of observed to expected emergency department visits for hypoglycemia among older adults (aged ≥67 years) with diabetes.
This measure reflects a key component of health plan quality pertaining to the management of diabetes, since older adults are more likely to experience severe hypoglycemia, potentially leading to several adverse outcomes: fall-related events and fractures, increased risk of cardiovascular events, and cognitive decline. Similarly, prevailing clinical practice guidelines for the treatment of older adults with diabetes emphasize the prevention of hypoglycemia as an important outcome. The new HEDIS measure provides an opportunity for health plans to identify older members with diabetes who are at highest risk of hypoglycemia and implement preventive interventions and more intensive management.
Learn MoreKey findings from the symposium at the Academy of Managed Care Pharmacy (AMCP) 2022 Annual Meeting.
Key Takeaways from Dr. Peek:
– rtCGM demonstrated a robust, sustained effect on glycemic control with fewer medications and no increase in insulin doses compared with
blood glucose monitoring (BGM) in the MOBILE RCT
– In the Kaiser analysis, rtCGM initiation reduced healthcare resource utilization for ER/admit due to hypoglycemia by 53%
– Expanded access to rtCGM is warranted based on these findings, particularly in underserved demographics disproportionately affected by
diabetes
Key Takeaways from Dr. Mistry:
– Pharmacy coverage of rtCGM for members with T1 and T2D can result in reduced resource utilization from improvements in clinical
management as well as cost savings for health plans via administrative efficiencies
-rtCGM offers an opportunity for improved outcomes
and proven PMPM savings when covered under the pharmacy benefit
Key Takeaways from Kelly Close:
– CGM represents the single most important tool for improving clinical outcomes and quality of life for people with diabetes
– The lives of people with diabetes have improved exponentially over the past several decades, but continued advancement is possible
with increased access to CGM and the application of more sophisticated measures such as TIR
Jointly provided by Impact Education, LLC, and Medical Education Resources.
This activity is supported by an independent educational grant from Dexcom, Inc.

The American Diabetes Association (ADA) Standards of Medical Care represent the latest evidence-based recommendations for guiding clinical practice. According to the most recent edition of these guidelines, Level A evidence from the MOBILE study supports the use of real time continuous glucose monitoring (rtCGM) in patients with insulin-treated type 2 diabetes (T2D) regardless of regimen. The findings from the MOBILE study likewise demonstrate the value of rtCGM across typically underserved demographics of patients impacted by social determinants of health (SDOH). Taking the ADA recommendations into consideration, payers are formulating coverage policies that facilitate appropriate access to rtCGM, improved outcomes in T2D, and proven per-member-per-month (PMPM) cost savings.
Video Summary


Source: The Journal of the American Medical Association
Authors: Monica E. Peek, MD, MPH, MS; Celeste C. Thomas, MD, MS
“…the studies by Karter et al. and Martens et al. provide additional evidence that patients with type 2 diabetes benefit from the use of CGM in terms of improved HbA1c level, time spent in the target blood glucose range, and reduced hypoglycemic episodes…”
“…institutional changes that promote its use in primary care will go a long way to improving diabetes control and reducing complications, particularly among the populations most in need. The time has come to broaden access to CGM for patients with type 2 diabetes.”
Learn More